Indians Need to Share Contraceptive Responsibility (GS Paper 2, Health)
Context
- As India continues to advance gender equality and rights, the idea of shared contraceptive responsibility between men and women must be normalized.
- Male sterilisation, particularly vasectomy, has a key role in reducing the disproportionate burden on women regarding family planning and contraception.
Introduction
India pioneered a national family planning program in 1952, initially aimed at improving maternal and child health. Over time, its focus shifted toward population stabilization. The methods of contraception have evolved, including a focus on permanent methods like sterilisation.
- 1966-70: During this period, 80.5% of sterilisation procedures were vasectomies.
- However, over the years, the focus on male sterilisation has diminished, and the percentage of vasectomies performed has steadily declined.
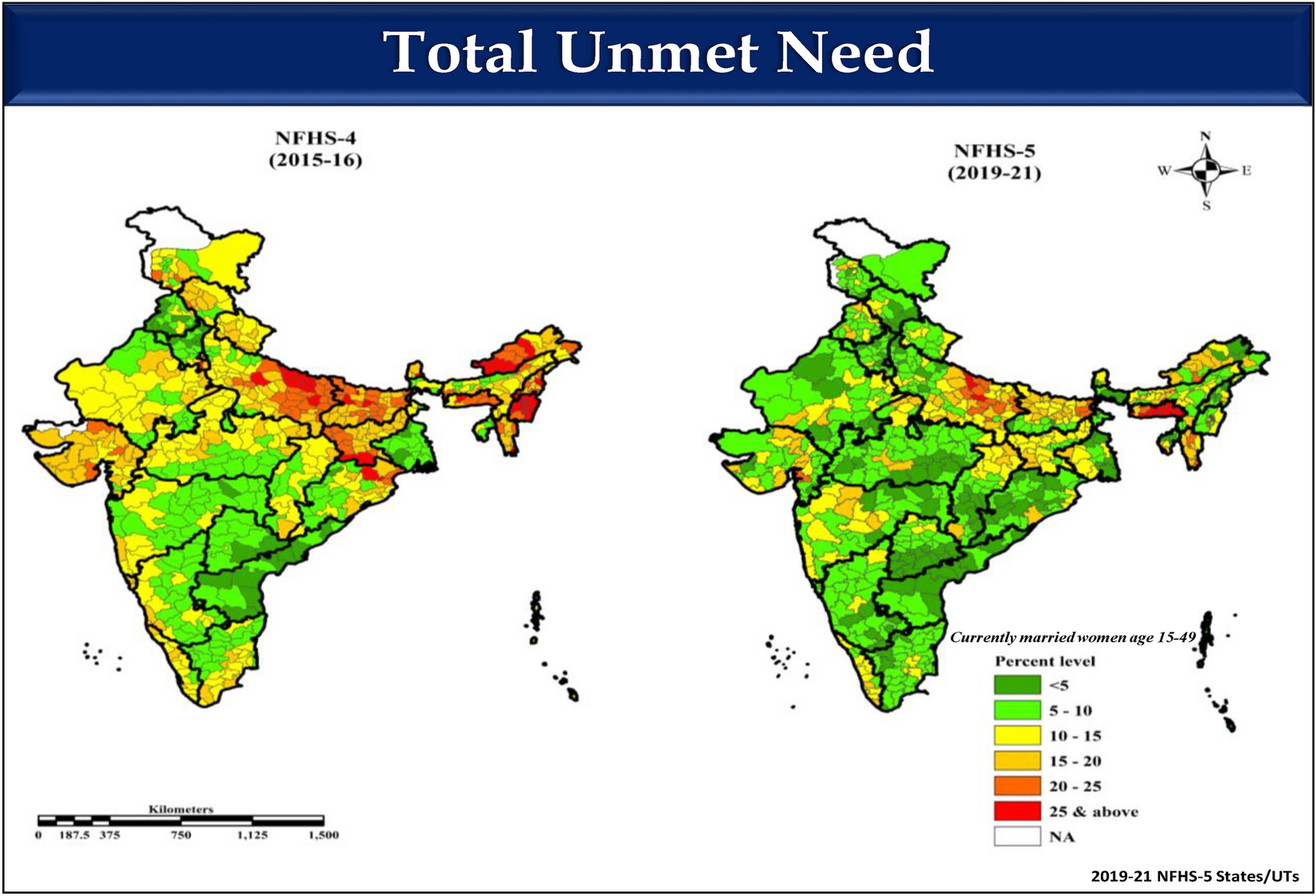
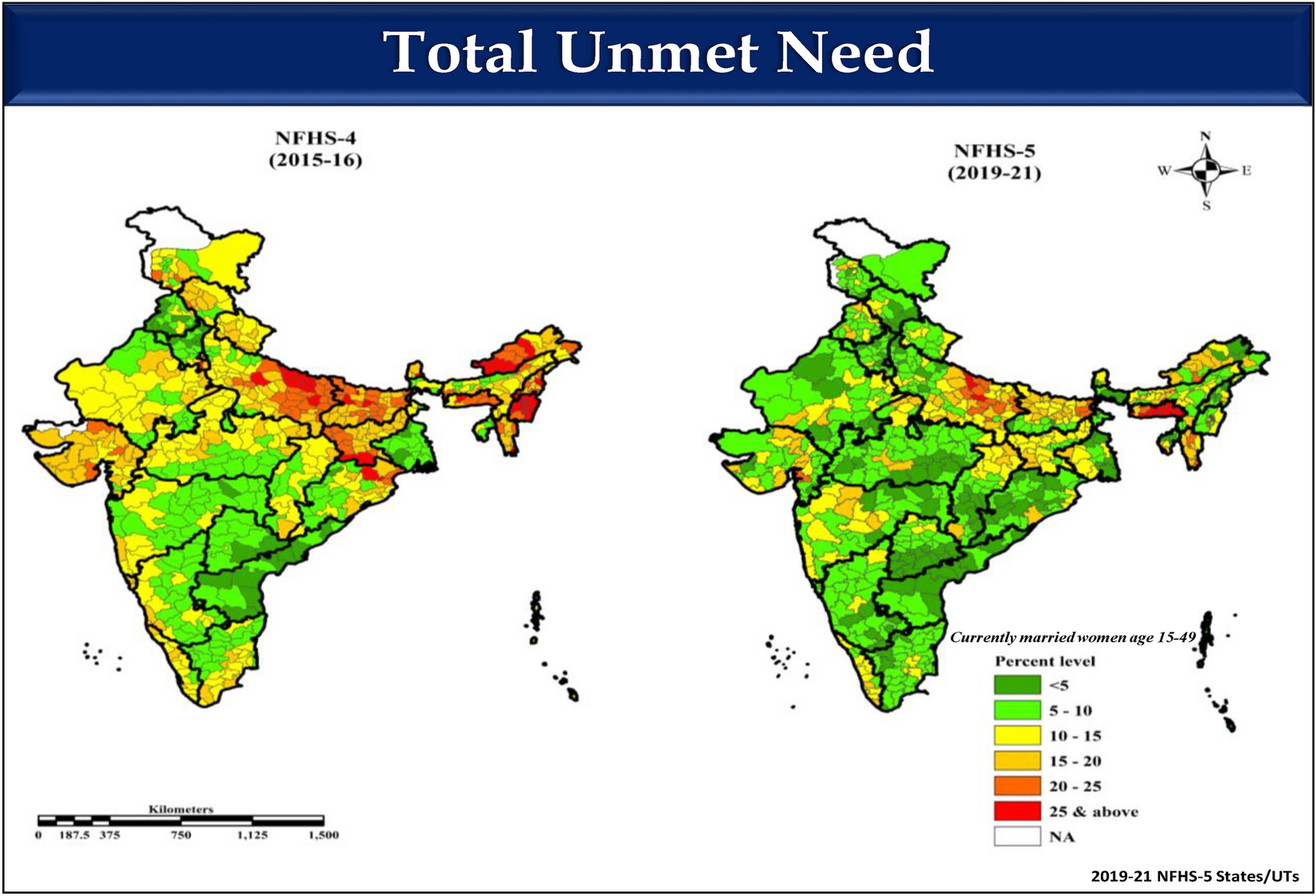
The National Family Health Survey (NFHS) data indicates that vasectomy use has stagnated in the last three decades, remaining at around 0.3% in NFHS-4 (2015-16) and NFHS-5.
Gender and the Disparity in Sterilisation Trends
- Policy Target: The National Health Policy 2017 aimed to increase male sterilisation to 30% of total sterilisation procedures. However, this target has not been achieved.
- Current Statistics: Data show a stark disparity:
- Female sterilisation: 37.9% of all sterilisation procedures.
- Male sterilisation: Only 0.3%.
This disparity indicates that women continue to bear the bulk of responsibility for permanent contraception, perpetuating gender inequality in reproductive health.
- This gender imbalance poses a challenge for achieving Sustainable Development Goal 5 — gender equality and the empowerment of women by 2030.
Awareness and Advocacy Initiatives
Efforts to address this issue include:
- Vasectomy Day: Observed on the third Friday of November, with the aim of increasing awareness about vasectomy and challenging misconceptions around it.
- Vasectomy Fortnight (2017): India launched an initiative to promote male sterilisation, aiming to increase awareness, debunk myths, and generate demand among men for vasectomies.
The goal of these advocacy efforts is to make vasectomies a more widely accepted option for men, especially those already seeking contraception or unaware of the safe alternatives available.
Ground Reality and Solutions
Insights from field surveys, like one conducted in Chhatrapati Sambhaji Nagar (Maharashtra, 2024), reveal the deep-rooted social attitudes affecting male sterilisation:
- Women’s Perspective: Many women in rural areas feel that sterilisation is their responsibility, with men reluctant to undergo vasectomies. Some view it as an additional burden on men, who already face economic hardships.
- Lack of Awareness: Many women are unaware of the financial incentives offered by the government for men undergoing vasectomies to offset wage loss.
- Misconceptions: Illiteracy, misconceptions about virility, and family opposition contribute to the low acceptance of vasectomies among men.
- Healthcare Challenges: The unavailability of skilled providers, especially in rural areas, has further limited the uptake of vasectomies. Many community health workers are unaware of the no-scalpel vasectomy technique, which is safer and less invasive.
With growing awareness of gender equality and rights, there is an opportunity to shift societal attitudes toward male sterilisation, making it more acceptable and commonplace.
Suggested Interventions
Adolescent Sensitisation:
-
- Begin education on family planning and sterilisation in early adolescence through school programs.
- This could lay the foundation for a future where vasectomy is seen as a shared responsibility.
- Use peer-group discussions and social media campaigns to debunk myths and destigmatise vasectomies.
Enhanced Financial Incentives:
-
- Increase conditional cash incentives for men undergoing vasectomies, especially in rural areas where the procedure is underutilised.
- A study in Maharashtra (2019) showed that incentives led to higher uptake in rural tribal communities.
Global Best Practices:
-
- Learn from countries where vasectomy uptake has been successful:
- South Korea has the highest prevalence of vasectomy, driven by progressive societal norms and gender equality.
- Bhutan popularised vasectomy through government campaigns and quality service delivery.
- Brazil increased vasectomy use through mass media campaigns, boosting the prevalence rate from 0.8% in the 1980s to 5% in recent years.
Conclusion
- To truly address the issue of gender equality in family planning, India must prioritize shared responsibility for contraceptive methods.
- Awareness campaigns, financial incentives, and education reforms can help shift societal attitudes toward male sterilisation.
- The government must also strengthen its healthcare infrastructure, ensure greater access to skilled providers, and improve training in non-scalpel vasectomies.
- Ultimately, policies should not only have good intentions but also clear, actionable steps for increased male participation in family planning.
- A demand-driven approach, alongside improved service delivery, is necessary for achieving gender equality and empowering women in India.